Expert Help for OCD
Take Your Life Back from OCD
Offering expert treatment for all types of OCD, including unwanted obsessional thoughts. Our OCD treatment program is typically 10 weeks. We offer twice-weekly sessions, groups, and intensive programs. Intensive program can be in person or online. Low cost options available. Contact us...
Behavioral Wellness Clinic
392 Merrow Rd, Suite E,
Tolland, CT 06084
Office: (860) 830-7838
OCDTYPES
Obsessive-compulsive disorder comes in many forms
Excoriation Disorder
Compulsive Skin-Picking is Also Called Dermatillomania
What Is Excoriation Disorder?
Excoriation Disorder is also called compulsive skin-picking, a body-focused repetitive behavior that results in the destruction of one's own skin. The face is usually the main target of skin picking, but compulsive skin-picking may involve any part of the body, often fingers, hands, and nails. Skin picking is a form of self-mutilation that can be quite serious, as people who suffer from Excoriation Disorder may experience bleeding, bruises, infections, scarring or even permanent damage to the skin. The behavior is often unconscious, and people with this compulsion may have difficulty stopping because they are often unaware of their actions. Excoriation Disorder is also called dermatillomania. It is classified by psychiatrists as an OCD-Related Disorder or even an impulse control disorder.

What Causes Compulsive Skin Picking?
The cause of compulsive skin-picking is probably a combination of biological and environmental factors. Many animals engage in excessive skin-picking and scratching, and some have theorized that an out-of-control grooming mechanism in the brain causes these behaviors. Scientists have developed mice who are missing a certain gene, causing them to engage in compulsive grooming that leads to bald spots and patches of missing fur. These behaviors may increase when under stress.
Compulsive skin-picking is often observed in people suffering from obsessive-compulsive disorder; in fact, about a quarter of those with OCD also have Excoriation Disorder. About a quarter of those with body dysmorphic disorder also have Excoriation Disorder. The most well-understood form of compulsive self-mutilation is trichotillomania or compulsive hair pulling, and this also tends to disproportionately afflict people with OCD. Because it is a repetitive behavior and common in people with obsessive-compulsive disorder, is considered to be related to OCD. These disorders tend to run in families.
There are several reasons why people with Excoriation Disorder continue their behaviors.
- Self-Soothing: When stressed, many people feel a need for self-soothing and find they feel better when they pick. Skin-picking has a kind of soothing effect on their nervous systems, and reduces over stimulation.
- Stimulation: On the other hand, when people are bored or inactive, skin-picking may provide a needed level of stimulation for the nervous system. It may help keep a person alert or awake when they would otherwise become bored or distracted.
- Perfectionism: Skin-pickers may stand for hours in front of mirrors closely examining their faces or other body areas for the tiniest irregularity and then try to fix it, in hopes of achieving a perfect complexion. Paradoxically, the skin-pickers always end up looking much worse in spite of their efforts, as a result of the damage that they do to themselves in the relentless pursuit of perfectionism.
Skin-picking can result in a self-perpetuating cycle. Picking may lead to shame and anxiety, which can result in more picking.
Treatment for Excoriation Disorder
Skin-picking can become a major focus of life and can interfere with relationships, work, and general happiness. Not recognizing the problem as a real disorder, many do not seek treatment. People with Excoriation Disorder may feel crazy and out of control, but not know what to do or where to go for help. Fortunately, Excoriation Disorder responds well to behavioral therapy.
Medication: The medications mainly used to treat skin-picking are the same group as those used for OCD, including antidepressants (SSRIs). Drugs that help skin-picking may take several weeks before they start working. They also may not work well. Usually, 65 percent improvement from a medication is considered a good result. Medication should never be considered an end in itself, but a tool to help with therapy.
Natural Remedies: Some people benefit from the B-vitamin inositol, which seems to reduce the urge to pull or pick. It is broken down by the body into two neurotransmitters that enhance the activity of serotonin in the brain. Serotonin, is a brain transmitter that may be implicated in OCD and related disorders.
Psychotherapy: Cognitive-behavior therapy has been studied as a means of treating skin-picking and related disorders. Therapy may involve several different techniques, outlined below:
- Habit Reversal Training (HRT) is a four-step process which teaches the person with how to relax, how to breathe and feel centered, and to perform muscle response exercises. HRT includes self-monitoring and stimulus control (described below) and social support.
- Self-Monitoring is simply making the person with Excoriation Disorder more aware of their behaviors. As the behavior can often be unconscious, awareness can be improved by simply keeping a log of picking behaviors. The very act of recording the behavior can also interrupt the process and reduce the picking.
- Stimulus Control (SC) is a behavioral treatment that helps sufferers identify and eliminate, avoid, or change the environmental factors, moods, or circumstances that trigger picking. The goal is to consciously control these triggers to create new learned connections between the urges and alternative, non-destructive behaviors. For example if picking usually occurs while alone, the person will be encouraged to spend more time with others. If the picking occurs in front of the mirror, then the person may be asked to cover the mirrors in their home.
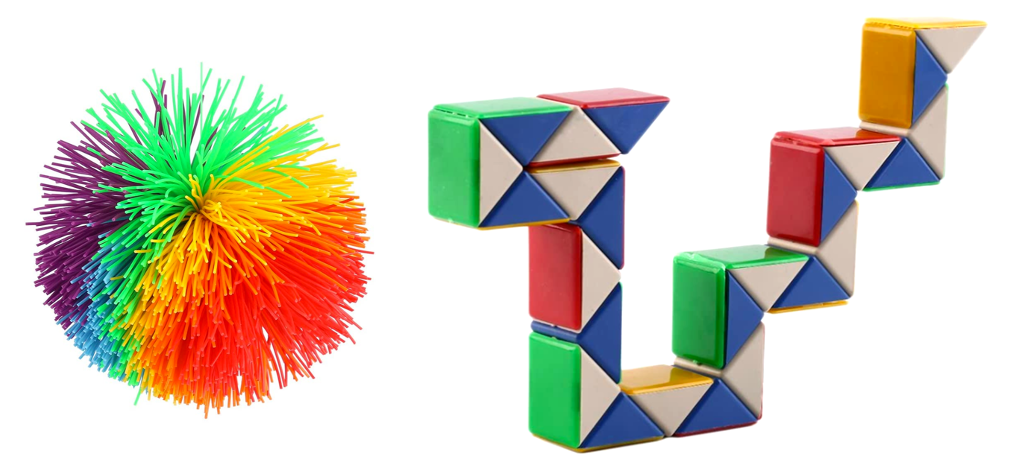
- Competing Response is a technique designed to give the person an alternative to picking. This can include fidget toys, knitting, beading, or other activities to keep the hands busy.
These techniques are all temporary means of helping the person learn to resist the urge to pick. The more the urge is resisted, over time the weaker the urge becomes. Once the urge fades, these techniques become less necessary. The length of time it takes to extinguish the behavior depends on how long the person has had the problem and how diligent they are in resisting the urges. Although therapy typically lasts from 10-12 weeks, it can take up to 12 months for the urge to pick to finally fade away.